Enormous drug company profits are the primary driver of soaring prescription drug prices in America, according to a damning investigation that Democrats on the House Oversight Committee began releasing Wednesday.
The first two reports in the investigation focus on Celgene and Bristol Myers Squibb’s Revlimid cancer treatment, which saw its price hiked 23 times since 2005, and Teva’s multiple sclerosis drug Copaxone, which went up in price 27 times since 2007.
Those costs have little to do with research and development or industry efforts to help people afford medication, as drug companies often claim, according to the probe.
“It’s true, many of these pharmaceutical industries have come up with lifesaving and pain-relieving medications, but they’re killing us with the prices they charge,” Rep. Peter Welch (D-Vt.) said as the hearings began Wednesday. He added that “uninhibited pricing power has transformed America’s pain into pharma’s profit.”
The top Republican on the committee, Rep. James Comer of Kentucky, called the investigation a partisan attack. “These hearings seem designed simply to vilify and publicly shame pharmaceutical company executives,” Comer said.
Much of the drug industry’s profits come at the expense of taxpayers and the Medicare program, are used to pay generous executive bonuses and are guarded by aggressive lobbying and efforts to block competition, regulation or systemic change in the United States while the rest of the world pays less, the reports say.
“The drug companies are bringing in tens of billions of dollars in revenues, making astronomical profits, and rewarding their executives with lavish compensation packages — all without any apparent limit on what they can charge,” committee chair Rep. Carolyn Maloney (D-N.Y.) wrote in a letter attached to the first two staff reports.
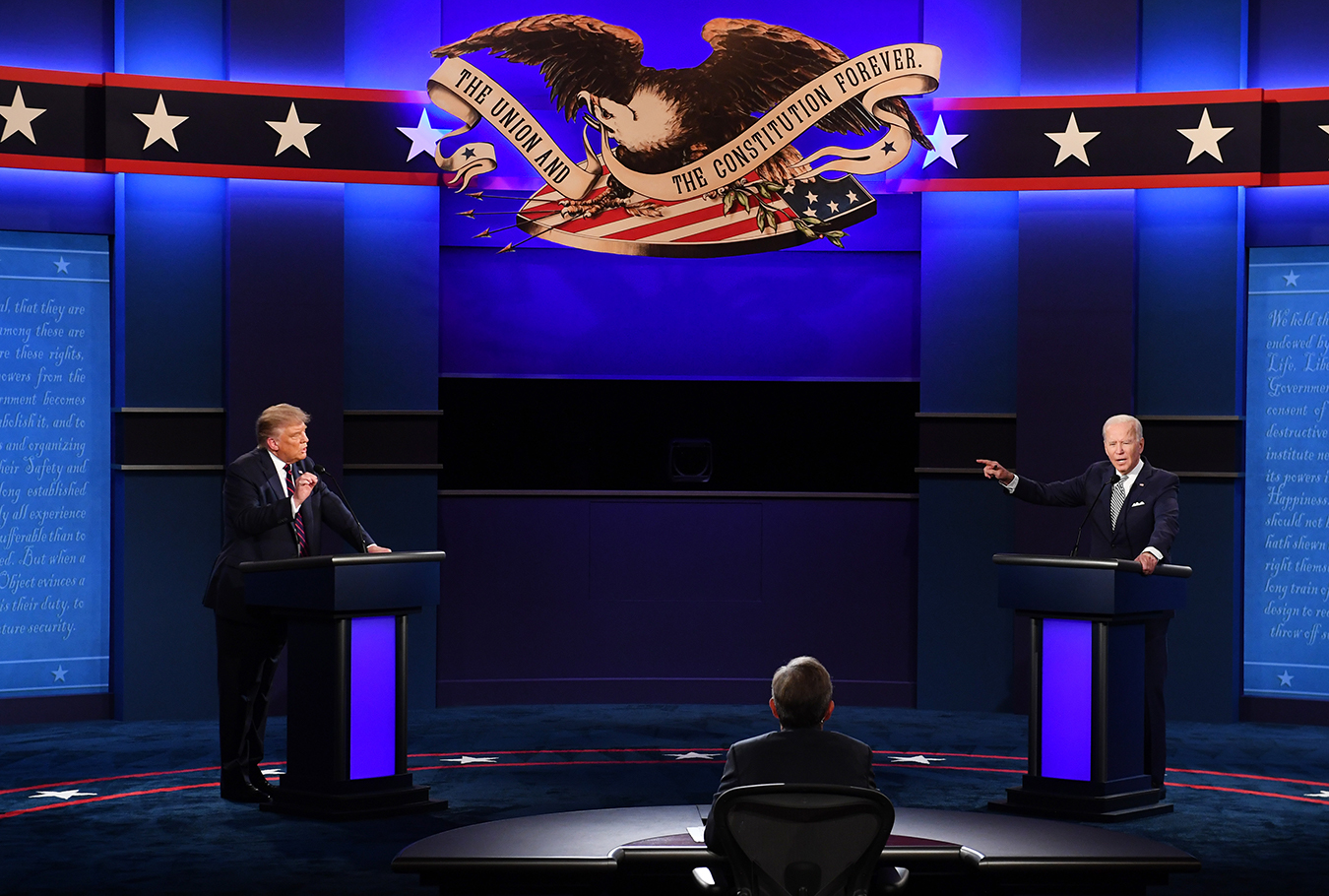
Rep. Elijah Cummings (D-Md.), the former committee chairperson who died last October, launched the probe more than a year ago. It has since produced more than a million documents. CEOs of Teva Pharmaceutical Industries, Celgene and Bristol Myers Squibb were testifying Wednesday.
Amgen, Mallinckrodt Pharmaceuticals and Novartis were scheduled to appear Thursday.
Celgene CEO Mark Alles verified the accuracy of the documents obtained by the committee and argued that the company’s pricing is entirely aboveboard and merited.
Rep. Katie Porter (D-Calif.) broke down the profits for Celgene in an especially personal way, telling Alles exactly how much of his $13 million compensation came from a bonus off Revlimid price hikes: $500,000, pegged to profits from that one drug.
Porter wrote the increasing prices for Revlimid on a whiteboard as she asked Alles if the drug got better over the years. He said it got approved for more uses, prompting Porter to shoot back that that meant more patients, not an improved drug.
“You received half a million dollars, personally, just by tripling the price of Revlimid,” Porter said. “To recap here, the drug didn’t get any better. The cancer patients didn’t get any better. You just got better at making money.” Porter noted that taxpayers spent $3.3 billion on Revlimid for Medicare beneficiaries.
(Source: House Committee on Oversight and Reform via Capitol News Forum)
Teva CEO Kåre Schultz demurred from addressing specific questions about much of the report, saying he took over only in 2017, in part to repair a company suffering after its Copaxone patent finally expired.
He also sounded the familiar refrain that prices are justified by research costs.
“In order for any pharmaceutical company to research and develop new drugs, or improve old ones, the price of successful medicines must reflect the significant cost of ongoing research and development projects,” Schultz said. “The public only sees and pays for the drugs that are ultimately approved by the government, like Copaxone, but you have to expend a lot of resources and endure many disappointments before bringing to the market safe and effective medicines.”
Maloney’s letter called the exorbitant price hikes for vital drugs “simply unsustainable,” and said she hopes the investigation spurs change.
Several themes common to pricing practices emerge in both reports, particularly aggressive pricing strategies that depend on the U.S. market and are divorced from underlying costs of manufacturing or development.
In the case of Revlimid, Celgene hiked the price from $215 per pill to $719 per pill when Bristol Myers Squibb gained the rights to it last year. The drug now costs $763 per pill, or $16,023 for a monthly course — more than three times the original cost in 2005.
In the case of Copaxone, Teva raised its price from less than $10,000 for a yearly course in 1997 to nearly $70,000.
Such price hikes have been predictably profitable. Teva has banked more than $34 billion in net profits in the United States alone, while Revlimid spun off $32 billion from the United States from 2009 to 2018 for Celgene. Medicare alone paid $17.5 billion for Revlimid from 2010 to 2018.
According to emails released with the reports, executives raised prices at will to meet quarterly profit goals, unrelated to costs. In one such case in 2014, then-Celgene executive vice president Mark Alles, who later became CEO, ordered up price hikes simply to juice flagging first-quarter numbers. “I have to consider every legitimate opportunity available to us to improve our Q1 performance,” Alles wrote. The first of two hikes was carried out less than a week later.
The investigation also undercuts the pharmaceutical industry’s claims that increased rebates, discounts and fees paid to pharmacy benefit managers drive prices. In the case of Revlimid, the largest discount Celgene ever paid in the commercial market was 5%, and the drug’s average net price after rebates, discounts and fees rose every year. Celgene’s Revlimid copay program cost just 0.16% of its net U.S. revenue from 2011 to 2018.
The average net price of Teva’s Copaxone similarly spiked every year until 2017 when a generic finally hit the market. Indeed, while Teva touted its patient assistance programs as a cost driver and a way to help people afford the drug, internally it described those efforts as a marketing ploy that spurred sales. For instance, the $70 million Teva spent on “Private Insurance Financial Assistance” yielded a 451% return on investment, internal documents show.
The oft-mentioned R&D also does not account for costs. In the case of Teva, it’s particularly glaring. Teva identified $689 million in development costs since 1989 — only about 2% of its U.S. profits from 2002 to 2019.
For Revlimid, the drug stemmed from basic research done in government-backed studies on thalidomide and related compounds. Celgene swooped in after the research showed the promise of the compound that would become Revlimid. And as it justified price hikes, Celgene’s internal documents cited the value of the drug, not the costs to develop it. To prove the value, it cited numerous research studies, many of which were done by others, including the National Institutes of Health.
While offering spurious rationales for raising prices, the companies worked hard to protect those prices, the investigation found. The most well-known are the aggressive lobbying tactics that the pharma industry deploys.
But there are many others, including using the high cost of the drugs themselves as a deterrent by making it extremely expensive for generic developers to buy enough samples for their own studies. In one case, Celgene used an FDA-required Risk Evaluation and Mitigation Strategy — which limits the distribution of risky drugs — to “prevent or delay 14 generic manufacturers from purchasing sufficient samples of Revlimid to obtain FDA approval,” the report on Celgene said.
The single-greatest step to curb prices, according to the report, would be to allow Medicare to negotiate prices. Both reports note how the companies highlight the noncompetitive U.S. market — specifically Medicare — as the means to ensure high profits.
For instance, the report says, “internal Teva documents warned that the legislative reform that posed the greatest threat to Teva’s future revenue was ‘Medicare Reform: Removal of government non-interference.’”
https://wp.me/p7iF68-SA0
#DrugCosts, #HealthCareCosts, #HealthIndustry, #Pharmaceuticals, #PrescriptionDrugs, #USCongress, #News

 17:36
17:36
 Annapoorna
Annapoorna